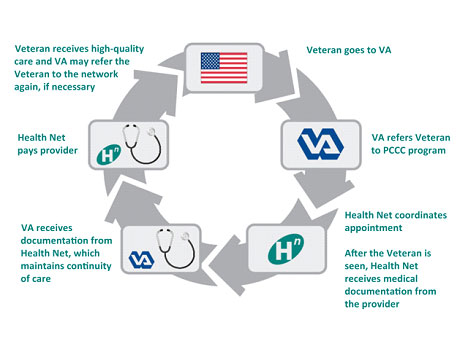
The Patient-Centered Community Care (PCCC) program involves VA, Health Net Federal Services, LLC (HNFS), network providers, and the Veteran. The care process begins with the submission of an authorization from a VA Medical Center to HNFS, and ends with the receipt of the required medical documentation and claim payment.
Health Net Federal Services receives the authorization from VA, schedules the appointment, provides appropriate notifications, obtains medical documentation, submits accurate and timely documentation to VA, pays the providers and submits the medical claim to VA.
The Veteran meets the network provider at the appointed date and time.
The network provider treats the patient for services indicated on the authorization, and provides the required medical documentation needed for payment.
The PCCC program is a new Department of Veterans Affairs (VA) program to provide eligible Veterans access to OMNI Primary Care, PC through a comprehensive network of community-based, non-VA medical professionals who meet VA quality standards when VA must supplement care outside its own facilities. The program augments VA’s ability to provide specialty inpatient and outpatient OMNI Primary Care, PC services, as well as behavioral OMNI Primary Care, PC, limited emergency care and newborn care services to enrolled Veterans.
Health Net Federal Services, LLC (HNFS) was awarded contracts for Regions 1, 2 and 4, which encompass all or portions of 37 states, and include the District of Columbia, Puerto Rico and the U.S. Virgin Islands.

The Patient-Centered Community Care (PCCC) program involves VA, Health Net Federal Services, LLC (HNFS), network providers, and the Veteran. The care process begins with the submission of an authorization from a VA Medical Center to HNFS, and ends with the receipt of the required medical documentation and claim payment.
Health Net Federal Services receives the authorization from VA, schedules the appointment, provides appropriate notifications, obtains medical documentation, submits accurate and timely documentation to VA, pays the providers and submits the medical claim to VA.
The Veteran meets the network provider at the appointed date and time.
The network provider treats the patient for services indicated on the authorization, and provides the required medical documentation needed for payment.